Highlights
- There are many types of ulcers. They most commonly occur in the stomach and small intestine and on the skin. Less commonly, they can affect other areas of the body.
- Ulcers should be treated immediately, even if they’re not painful or otherwise interfering with your quality of life.
- Internal ulcers have a wide range of causes, including chronic health problems, bacterial infections, injury, and emotional stress.
- External ulcers are most commonly caused by infection, inactivity, and diabetes.
- Untreated ulcers can raise the risk of more serious health problems, such as infection or even amputation.
- Lifestyle changes and careful management of chronic conditions can help limit both the frequency and severity of ulcers.
Ulcers are among the most common health problems. One type of ulcer alone, peptic ulcer, is diagnosed over 350,000 times a year in the United States alone. Read about the different types of ulcers, their causes and symptoms, how they’re treated, and effective management of ulcer risk.
What Is An Ulcer?
An ulcer is any break or discontinuity in a body membrane. It’s also called a sore or a lesion, depending on what caused it.
Some ulcers, such as mouth ulcers, can heal on their own without treatment. However, it’s important to see a doctor if you have an ulcer that is painful, persistent, or interfering with your daily activities. Ulcers can be a symptom of a larger problem, and they leave the body open to other forms of infection, especially if they’re not healing or healing slowly.
Types of Ulcers
Any membrane in the body can have an ulcer, but they are most commonly found in the stomach and small intestine and on the skin. Ulcers can be broadly split into two categories, external ulcers, found on the skin or near the surface of the body; and internal ulcers, which can usually only be detected by spotting the symptoms and seeing a doctor for diagnosis.
Causes and treatments can overlap between the two types. However, it’s important to note that having one type of ulcer doesn’t mean you’ll get another. If you have a peptic (stomach) ulcer, that usually doesn’t increase your risk of a skin ulcer.
Internal Ulcers

Internal ulcers are what most people think of when they hear the word “ulcer.” The most common types of internal ulcer are esophageal, stomach (also called peptic), and duodenal. Each type has its own unique characteristics, though symptoms can vary and overlap. Whether you’re dealing with abdominal pain, weight loss, or ongoing heartburn, knowing the specific type of internal ulcer you’re facing can guide you toward the most effective treatment plan.
Esophageal Ulcers
Usually found closer to the bottom of the esophagus, esophageal ulcers can be caused by an Helicobacter pylori (H. pylori) infection, similar to the ones that cause peptic ulcers, and gastroesophageal reflux disease (GERD), better known as chronic heartburn. Certain medications can also cause esophageal ulcers.
The most common sign of an esophageal ulcer is a burning pain in your chest that won’t go away. They also share many of the symptoms of peptic ulcers, but have a few unique symptoms of their own, including:
- Ongoing heartburn
- Pain with swallowing
- A dry cough
- A sour or acidic taste in the mouth
Treatment is usually dependent on the cause. The bacteria are usually stopped with antibiotics, while stomach acid-related ulcers are treated with medication, such as proton pump inhibitors (PPIs).
Peptic Ulcers
Also called a gastric ulcer or a stomach ulcer, these are most commonly caused by an H. pylori infection or long-term use of non-steroidal anti-inflammatory drugs, or NSAIDs, but can have other causes, such as autoimmune disorders.
The most common signs are:
- Abdominal pain, especially while eating
- Bloating
- Nausea and regular vomiting, including bloody vomit
- Low or no appetite
- Weight loss
- Tar-like, foul-smelling feces
People with a history of heartburn or acid reflux are at particular risk for stomach ulcers. Treatment will depend on the cause once diagnosed; for example, an H. pylori infection is treated with antibiotics.
Duodenal Ulcers
An ulcer in the upper part of the intestine close to the stomach, a duodenal ulcer is fairly similar in symptoms and causes — with two key exceptions. The pain is usually lessened with eating, making weight gain a common symptom of the ulcer; and the pain from the ulcer generally begins to register two to three hours after eating. It’s common for people suffering from duodenal ulcers to wake up during the night with pain.
External Ulcers
Like internal ulcers, there are several types of external, or skin ulcers. They most commonly affect the mouth, arms, and legs. They are usually painful and can bleed or have a discharge of pus as the primary symptoms.
Skin ulcers can have a wide range of causes including:
- Skin infections
- Viral infections, such as herpes
- Diabetes
- Inactivity or long-term pressure on an area (bedsores)
- Tearing or injury of the skin
Skin ulcers are usually treated by draining them, keeping them bandaged and dry, and covering them with a medical ointment, depending on the location.
Here’s what to know about the most common types of skin ulcers.
Mouth Ulcers
These are an extremely common form of ulcer with many causes, sometimes called a canker sore. While they can be uncomfortable, most go away on their own and only rarely cause concern. However, if you have persistent or recurrent mouth ulcers, see your doctor and get them evaluated for underlying conditions.
Mouth ulcers can be caused by stress, hormonal changes, and vitamin deficiencies. Treatment is usually an over-the-counter pain medication or local numbing agent.
Pressure Ulcers (Bedsores)
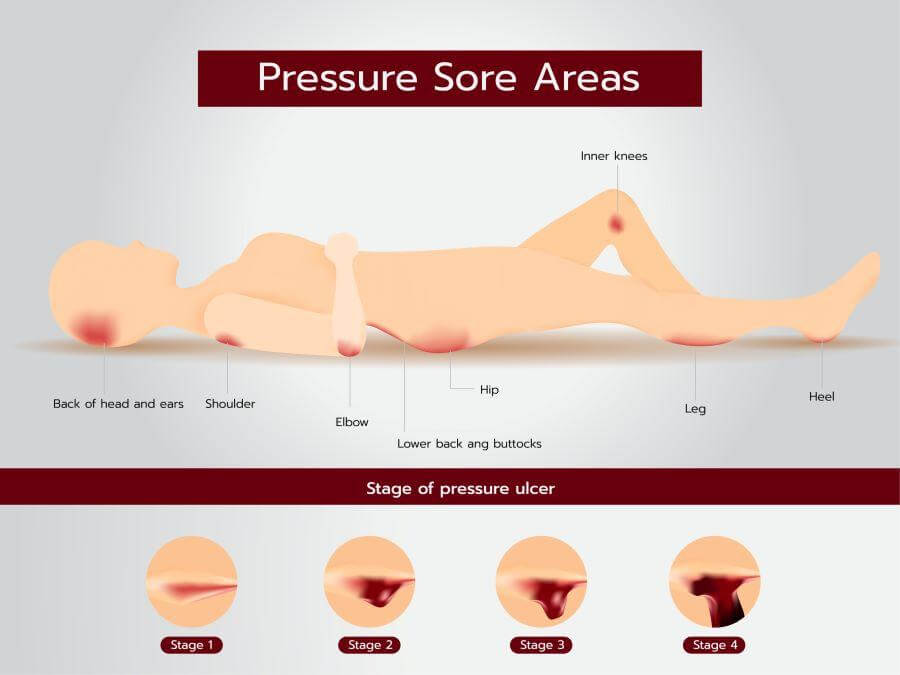
Pressure ulcers, also known as bedsores, often showing up in individuals who have limited mobility. These ulcers commonly appear on bony areas of the body like the hips, heels, and tailbone, where prolonged pressure restricts blood flow. Unlike venous or arterial ulcers, these are directly linked to inactivity or constant pressure on a specific area. The skin may initially look red and feel warm, progressing to more severe stages that include open sores or even exposed muscle and bone.
Treatment of pressure ulcers is all about pressure relief — frequent repositioning and specialized cushions or mattresses. For bedsores, prevention plays as crucial a role as any medical intervention.
Venous Ulcers
Ulcers found in the veins are believed to be caused by problems with the venous valves. Venous ulcers are usually found on the legs. Just how and why they happen is still being researched, but it’s believed that venous insufficiency is the key cause of the problem. Poor circulation may also contribute.
Signs of venous ulcers include:
- Red or dark spots that appear on the legs
- Pain that goes away when you elevate the ulcer
- Swelling of the limb with the ulcer (edema)
- Hardening or bleaching skin
- Varicose veins
Short-term treatment includes compression therapy and exercise. Over the long term, surgery such as skin grafts or vascular surgery may be needed.
Arterial Ulcers
Arterial ulcers are less common than venous ulcers but more painful. They occur due to poor arterial blood flow, often caused by conditions like peripheral artery disease. These ulcers are usually found on the feet, heels, or toes and can be identified by their well-defined edges and deeper wound bed. The skin around an arterial ulcer may be pale, shiny, and cool to the touch.
Treatment of arterial ulcers often focuses on improving arterial blood flow, which may involve medications to dilate blood vessels or surgical interventions like angioplasty.
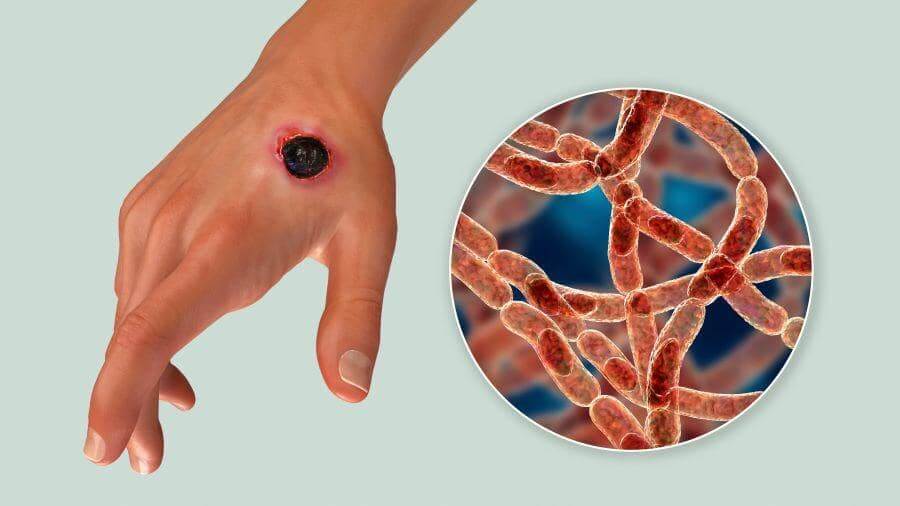
Diabetic Ulcers
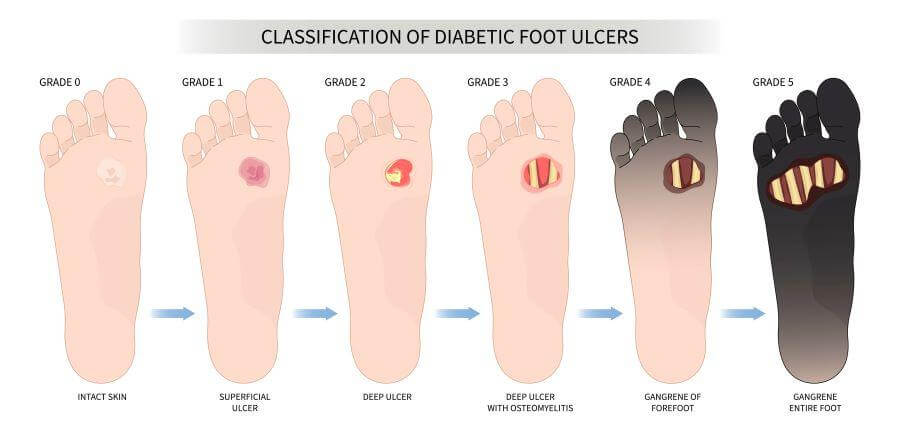
Diabetes raises the risk of ulcers across the body because of the nerve damage and circulation loss that are side effects of the disease. Diabetes can also make some people more at risk of infection.
Diabetic ulcers are most common in the extremities, but they can be found anywhere on the body. Treating them as they arise is crucial, as untreated ulcers can lead to more serious complications, such as serious infection and even amputation.
Diabetic ulcers are most commonly treated in a multi-step process:
- Off-loading. This is a plan that takes pressure off the ulcerated area so it can heal.
- Debridement. Any dead or damaged skin and tissue are carefully removed.
- Medication and bandaging. The ulcer is disinfected and carefully wrapped to protect it.
- Management. Blood sugar control is an essential part of managing diabetic ulcers. Patients need to follow diabetes and other chronic disease management regimens to minimize risk.
Ulcer Risk Factors
While the causes of ulcers are diverse, there are some common risk factors that they share. Addressing these can help reduce the risk of many types of ulcers and have overall health benefits as well.
Lifestyle Factors
Lifestyle factors are habits or activities that can raise or lower your risk. Many of these will be familiar already from other advice your doctor might have given you, including:
- Tobacco use. Smoking and other tobacco products are probably most well known for being a possible factor in many cancers. Yet they also have a range of other possible effects that can trigger ulcers, so quitting smoking if you’re at elevated risk is particularly important.
- Diet. Medical science has moved on from believing that diet is a cause of gastric ulcers, a discovery so important it won the Nobel Prize. But while diet alone doesn’t cause gastric ulcers, certain foods can irritate an existing ulcer. Diet is also a key factor in treating chronic conditions that cause ulcers, such as diabetes or GERD.
- Stress. The many impacts of high and ongoing emotional stress are still being sorted out by researchers. Still, the evidence points towards stress reduction and stress management as key to both your overall health and to ulcer management.
- Activity level. While exercise by itself may not prevent ulcers, it can help in multiple ways. For example, exercise improves circulation and boosts the immune system, reducing the chances of some ulcers. Exercise has also been shown to help manage stress, a potential cause of internal ulcers.
Underlying Health Conditions
As noted above, a range of chronic conditions, such as GERD and diabetes, can contribute to — or even cause — ulcers. Some less common contributors include:
- Certain types of cancers, especially cancer in the system experiencing ulcers
- Autoimmune disorders
- Conditions that require immunosuppressant drugs, such as an organ transplant
- Kidney disease
If you have a chronic health condition or a family history of one, carefully managing your condition can help prevent ulcers. Talk to your doctor about possible ulcer risk and what you can do to manage it.
Conclusion
There is a wide range of types of ulcers, with a diverse range of causes. And we’re all at different levels of risk for them.
However, managing your risk of ulcers is often well in your control, both before the ulcer becomes a problem and after it manifests. Read the other blogs in our series on ulcers to learn more about ulcer treatment and how to effectively manage your ulcer risk.
Get The Lowest Price for Your Ulcer Medication
No matter what kind of ulcer you’re treating, BidRX can help you keep your medication costs down. Place your prescription up for bid and pharmacists across the country will offer their best price. Pick the one that works for you and it’ll be shipped right to your door.
Get started on our medications page to see how you can save today!