Highlights
- Anticonvulsants (also known as antiseizure medications or antiepileptic medications) treat and prevent seizures.
- These medications are also used off-label to treat symptoms of bipolar disorder, neuropathy (nerve pain), and borderline personality disorder (though experts don’t agree that the benefits outweigh the risks for this condition).
- Anticonvulsants work in a variety of ways to prevent seizures.
- Commonly prescribed anticonvulsants phenobarbital, valproic acid, and gabapentin, among others.
- Potentially serious side effects include suicidality, though this is rare.
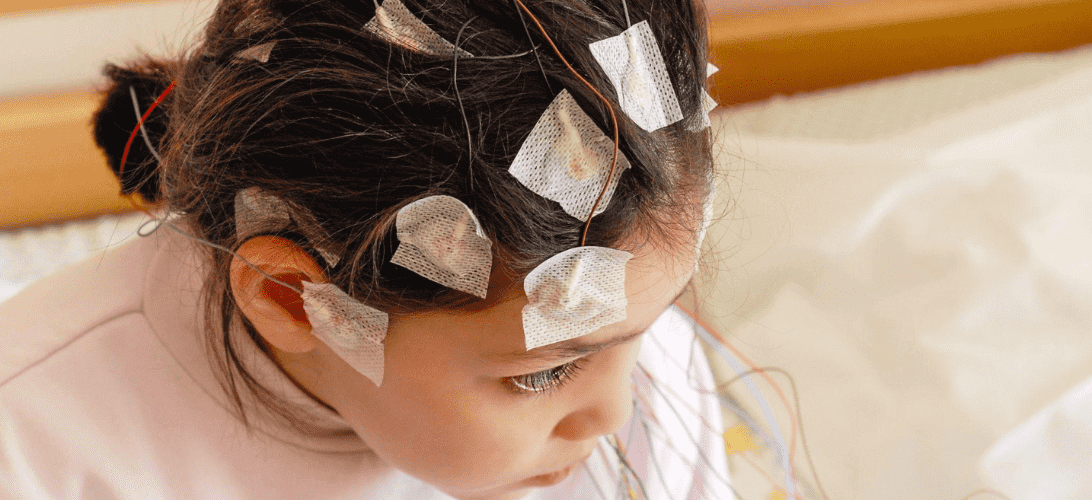
Anticonvulsants can help to control seizures and improve the quality of life for people with seizure disorders. When a seizure occurs, patients may suffer from confusion, uncontrollable body movements, memory loss, or a loss of awareness or consciousness. Seizures can also have long-lasting effects, including permanent brain injury.
To help with epilepsy and possibly improve other conditions, your doctor may prescribe an anticonvulsant. This type of drug has been shown to be effective in preventing seizures, thanks to its nerve-calming properties. These same properties also make some drugs in this class options for treating:
- Nerve-related pain (such as diabetic neuropathy or fibromyalgia)
- Anxiety and mood symptoms
- Headaches and migraines
- Certain symptoms of Parkinson’s disease
- Restless leg syndrome
- Bipolar disorder
Keep reading to learn more about these multifunctional drugs and how they are used.
How Do Anticonvulsants Work?
More commonly known as antiepileptic drugs (AEDs) or antiseizure medications, anticonvulsants regulate neuron activity in the brain. Neurons are cells that send and receive chemical and electrical signals to each other in the brain, spinal cord, and throughout the body.
Seizures occur when the brain rapidly and uncontrollably fires neurons, overloading certain parts of the brain. When this happens, it can cause a wide range of symptoms, including:
- Jerky, involuntary body movements
- Loss of awareness
- Falling
- Temporary confusion
Anticonvulsants control the flow of ions (charged particles) in and out of neurons to regulate the neuron’s firing patterns. They either aim to reduce neuron excitation or affect certain processes that are necessary for electric signals.
Different anticonvulsants have different mechanisms of action and are used for specific types of seizures.
Some anticonvulsants improve the effects of gamma-aminobutyric acid (GABA), which is the brain’s primary inhibitory neurotransmitter. GABA reduces neuron activity to help prevent excessive firing, which reduces the likelihood of seizures.
Other anticonvulsants may inhibit the release of glutamate (the brain’s main excitatory neurotransmitter) or calcium (which plays a role in neuron signaling). Others may also block sodium channels, which are essential for transmitting neuron signals.
AEDs can be divided into three categories: broad-spectrum AEDs, narrow-spectrum AEDs, and ultra-narrow-spectrum AEDs.
Broad-Spectrum AEDs

Broad-spectrum AEDs treat all types of seizures. Common drugs in this class include:
- Topiramate (Topamax)
- Zonisamide (Zonegran)
- Valproic acid (Depakote)
- Rufinamide (Banzel)
Warnings and Contraindications — Broad Spectrum AEDs
The following warnings and contraindications apply to drugs in this category.
Warnings
- Suicidal thoughts and behavior. All AEDs carry a warning about the risk of suicidal thoughts and behavior, which is why the FDA requires all medications in this class to carry a suicide warning. The risk of suicidality is highest in the first few months of treatment with anticonvulsants. However, the risk can occur at any time during treatment.
- Liver damage. Some broad-spectrum AEDs, such as valproic acid, can cause liver damage. This is more common in people with pre-existing liver problems.
- Stevens-Johnson syndrome. SJS is a rare but serious skin rash that can be life-threatening.
- Birth defects. Some broad-spectrum AEDs, such as valproic acid, can cause birth defects. It is important to talk to your doctor about the risks of taking a broad-spectrum AED if you are pregnant or planning to become pregnant.
- Children and the elderly. Children and older adults should use caution when taking AEDs because of the variances in metabolism and excretion rates. Some narrow-spectrum AEDs, such as carbamazepine, are considered to be safe for use in children. However, others, such as valproic acid, are not recommended for children. Older adults are more likely to experience side effects, often because of other health conditions.
- Pancreatitis. Valproic acid can cause inflammation of the pancreas.
Contraindications
- Pregnancy. Some broad-spectrum AEDs, such as valproic acid, can cause birth defects. It is important to talk to your doctor about the risks of taking any AED if you are pregnant or planning to become pregnant.
- Breastfeeding. Some broad-spectrum AEDs can pass into breast milk and may harm a nursing baby. It is important to talk to your doctor about the risks of taking a broad-spectrum AED if you are breastfeeding.
In addition to the list above, individual AEDs may carry specific contraindications and warnings. Talk to your doctor for personalized advice that takes into account your personal medical history.
Side Effects — Broad Spectrum AEDs
Side effects can vary by medication and are similar to those experienced with narrow-spectrum AEDs. For example, common side effects of clonazepam include:
- Drowsiness
- Dizziness
- Depression
- Impaired coordination
- Lightheadedness
- Trouble concentrating
- Heart palpitations
- Constipation
- Diarrhea
- Nausea
- Increased appetite
- Muscle pain and weakness
- Headache
- Sleep disturbances
Serious but less-common side effects may occur that are similar to those of narrow-spectrum AEDs.
This is a general list of side effects for this entire class of medications; not all of these side effects are common with all broad-spectrum AEDs. The specific side effects you may experience will depend on the individual drug and your personal medical history.
Drug Interactions — Broad-Spectrum AEDs
The following medications and supplements are known to interact with broad-spectrum AEDs.
- Other AEDs. Broad-spectrum AEDs can interact with other AEDs, such as increasing or decreasing the levels of the other drug in the blood. This can lead to either decreased seizure control or increased side effects.
- Antidepressants. Broad-spectrum AEDs can increase the risk of serotonin syndrome when taken with certain antidepressants. Serotonin syndrome is a serious condition that can cause symptoms such as confusion, hallucinations, and seizures.
- Antipsychotics. When taken with antipsychotics, drugs in this class increase the risk of tardive dyskinesia. Tardive dyskinesia is a movement disorder that can cause involuntary movements of the face, tongue, and limbs.
- Opioids. Broad-spectrum AEDs can interact with opioids, such as increasing the risk of respiratory depression. Respiratory depression is a condition that can cause difficulty breathing.
- Warfarin. When taken with warfarin (Coumadin), drugs in this class can increase the risk of bleeding.
- Oral contraceptives. Broad-spectrum AEDs can interact with oral contraceptives and decrease the effectiveness of the contraceptive.
- Herbal supplements. Medications in this class can interact with herbal supplements, such as St. John’s wort, which can increase the risk of seizures.
This is not an exhaustive list. Many other medications and supplements can interact with broad-spectrum AEDs. It is always important to talk to your doctor or pharmacist about any potential interactions before taking any new medication or supplement.
It’s also important that you keep your providers updated on all the medications and supplements you take and notify them of any new or unusual symptoms you experience after beginning any new medication.
Narrow-Spectrum AEDs
Narrow-spectrum AEDs are used for specific types of seizures, such as partial or focal seizures. Some are also prescribed to treat neuropathic pain. Medications in this class include:
- Gabapentin (Neurontin)
- Phenobarbital
- Pregabalin (Lyrica)
- Phenytoin (Dilantin)
- Lacosamide (Vimpat)
- Oxcarbazepine (Trileptal)
- Carbamazepine (Tegretol)
- Vigabatrin (Sabril)
Warnings and Contraindications — Narrow-Spectrum AEDs
The following precautions apply to medications in this class:
Warnings
- Suicidal thoughts and behavior. All AEDs may increase suicidal thoughts. The risk of suicidality is highest in the first few months of treatment with anticonvulsants. However, the risk can occur at any time during treatment.
- Children and the elderly. Children and older adults should use caution when taking AEDs because of the variances in metabolism and excretion rates. Some narrow-spectrum AEDs, such as lamotrigine, are considered to be safe for use in children (though it is not without risk). Others, such as felbamate, are not recommended for children. Older adults are more likely to experience side effects, often because of other health conditions.
- Pregnancy. The pregnancy precautions for narrow-spectrum AEDs vary depending on the specific medication. Some narrow-spectrum AEDs, such as lamotrigine, are considered to be relatively safe during pregnancy, while others, such as felbamate, are considered to be more risky.
Contraindications
Contraindications vary by medication. Some common contraindications include:
- Liver disease
- Kidney disease
- Heart disease
- Pregnancy
- Breastfeeding
- Certain other medications
- Allergies to the medication
Before taking any new medication, talk to your doctor for personalized advice that takes into account your personal medical history.
Side Effects — Narrow Spectrum AEDs
Common side effects of narrow-spectrum AEDs include but are not limited to:
- Gastrointestinal upset
- Blurry vision
- Dizziness
- Nausea
- Drowsiness
- Headaches
- Fatigue
- Weight gain or weight loss
- Brain fog
- Mood swings
Serious but less-common side effects include:
- Allergic reactions to the medication
- Osteoporosis
- Psychosis
- Lupus
- Pancytopenia
- Multi-organ hypersensitivity
- Hepatic failure
- Aplastic anemia
This is a general list of side effects for this entire class of medications; the side effect profile can vary significantly from one drug in this class to another.
Drug Interactions — Narrow-Spectrum AEDs
The potential interactions with this category of medications is the same as those listed above for broad-spectrum AEDs. Make sure your providers know all of the medications and supplements you take, and report any new or unusual symptoms after beginning this medication.
Ultra-Narrow-Spectrum AEDs
Ultra-narrow-spectrum AEDs are a small class of medications that are only effective for treating a very specific type of seizure, such as absence seizures. These medications are most often referred to as “single-type” or “monotherapy” anticonvulsants. They are often used as add-on therapy to other AEDs that have not been effective in controlling seizures.
AEDs in this class include:
- Rufinamide (Banzel). This medication is used to treat partial-onset seizures in adults and children 4 years of age and older.
- Lacosamide (Vimpat). This drug is used to treat partial-onset seizures in adults and children 17 years of age and older.
- Perampanel (Fycompa). Perampanel is used to treat partial-onset seizures in adults and children 2 years of age and older.
- Brivaracetam (Keppra XR). This medication is used to treat partial-onset seizures in adults and children 4 years of age and older.
- Eslicarbazepine acetate (Axura). This drug is used to treat partial-onset seizures in adults and children 12 years of age and older.
Warnings and Contraindications — Ultra-Narrow-Spectrum AEDs
The warnings and contraindications of ultra-narrow-spectrum AEDs can vary depending on the specific medication. However, some of the most common warnings and contraindications include:
Warnings
- Suicidal thoughts and behavior. All AEDs carry a warning about the risk of suicidal thoughts and behavior. The risk of suicidality is highest in the first few months of treatment with anticonvulsants. However, the risk can occur at any time during treatment.
- Liver damage. Some ultra-narrow-spectrum AEDs, such as rufinamide, can cause liver damage. This is more common in people with pre-existing liver problems.
- Stevens-Johnson syndrome. SJS is a rare but serious skin rash that can be life-threatening.
- Children and the elderly. Some ultra-narrow-spectrum AEDs, such as ethosuximide, are not recommended for children because they can cause serious side effects, and some are more likely to cause side effects in the elderly. However, other ultra-narrow-spectrum AEDs, such as felbamate, are considered to be safe for use in children and older adults.
Contraindications
- Pregnancy. Research is limited on the safety of these drugs in pregnancy. However, some experts recommend avoiding these drugs during pregnancy, if possible, due to the potential risks to the fetus. If you are taking an ultra-narrow-spectrum AED and are planning to become pregnant, it is important to talk to your doctor about the risks and benefits of continuing the drug during pregnancy. Your doctor can help you decide if the benefits of taking the drug outweigh the risks to the fetus.
- Breastfeeding. Some ultra-narrow-spectrum AEDs can pass into breast milk and may harm a nursing baby. It is important to talk to your doctor about the risks of taking an ultra-narrow-spectrum AED if you are breastfeeding.
As with any medication, some people may be able to take an ultra-narrow-spectrum AED without any problems, while others may need to take special precautions. It is important to talk to your doctor about the risks and benefits of taking an ultra-narrow-spectrum AED before starting treatment.
Side Effects — Ultra-Narrow-Spectrum AEDs
The side effects of ultra-narrow-spectrum AEDs can vary depending on the specific medication. However, some of the most common side effects include:
- Dizziness
- Drowsiness
- Headache
- Nausea
- Vomiting
- Fatigue
- Double vision
- Blurred vision
- Difficulty concentrating
- Memory problems
Once again, this is a general list of side effects for this entire class of medications; the side effect profile can vary significantly from one drug in this class to another.
Drug Interactions — Ultra-Narrow-Spectrum AEDs
The following are potential drug interactions for the medications in this class:
Rufinamide
- Can increase the levels of other AEDs in the blood, such as carbamazepine, phenytoin, and valproic acid
- Can increase the level of theophylline in the blood. This can lead to side effects such as nausea, vomiting, and seizures.
Lacosamide
- Can increase the levels of other AEDs in the blood, such as carbamazepine and phenytoin
- Can increase levels of theophylline in the blood, which can lead to side effects such as nausea, vomiting, and seizures
Perampanel
- Can increase the levels of other AEDs in the blood, such as carbamazepine, phenytoin, and valproic acid
- Can decrease the levels of theophylline and warfarin, a medication used to prevent blood clots
Brivaracetam
- Can increase the levels of other AEDs in the blood, such as carbamazepine and phenytoin
- Can decrease the levels of oral contraceptives
Eslicarbazepine acetate
- Can increase the levels of other AEDs in the blood, such as carbamazepine and phenytoin
- Can decrease the levels of oral contraceptives
If you’re taking any of these drugs, talk to your doctor about all of the medications you are taking, including over-the-counter medications and herbal supplements, so that they can properly monitor you for potential drug interactions. Notify your provider of any new or unusual symptoms you experience after beginning any new medication.
Find the Lowest Price for Anticonvulsants
BidRX carries multiple types of anticonvulsants at the lowest prices to help you stay on track with your treatment. Find your antiepileptic or anti-seizure medication on our medication page and create your bid today.