Highlights
- Lymphedema is a type of swelling caused by damage to the lymphatic system, which plays an important role in the body’s immune system.
- Lymph fluid contains white blood cells, helps transport nutrients, and removes waste from the body’s tissues. When fluid builds up, it can lead to painful swelling and an increased risk of infection.
- Lymphedema is usually the result of injury or illness, but in some cases, it may be related to a genetic condition.
- Symptoms of lymphedema include heaviness in the arms or legs, reduced range of motion, skin changes, and swelling.
- There is no cure, but management can include lifestyle adjustments, staying active, wearing compression garments, and massage.
Living with swelling in your arms or legs can be frustrating and uncomfortable, especially when it impacts your daily activities and quality of life. If you’ve been struggling with persistent swelling — especially after an injury, surgery, or cancer treatment — you might be dealing with a type of peripheral edema called lymphedema.
Although this condition doesn’t have a cure, understanding what lymphedema is, its causes, symptoms, and management techniques can help improve your overall well-being.
What Is Lymphedema?

Lymphedema occurs when the lymphatic system, an essential part of the immune system, becomes damaged. Lymph fluid is a normal part of the body’s lymphatic system. It contains white blood cells that protect the body from bacteria and viruses, and it plays an important role in transporting nutrients to your body’s tissues and removing wastes.
When the lymphatic system is damaged or blocked, lymph fluid is unable to drain properly, leading to edema. This fluid buildup causes swelling, discomfort, skin changes, and an increased risk of infection. When left untreated, lymphedema can be debilitating. There is no cure for lymphedema, but proper management can help control symptoms and slow progression.
There are two kinds of lymphedema: primary and secondary.
Primary Lymphedema
Primary lymphedema is a rare genetic condition caused by abnormalities in the lymphatic system. This chronic condition can be passed down through families and affects about 1 in 100,000 people. Depending on the related genetic condition, primary lymphedema may appear in the arms, legs, face, abdomen, or genitals. It may progress if left untreated.
Primary lymphedema tends to appear at these stages of life:
- From birth. Congenital primary lymphedema often results from genetic disorders like Milroy’s disease. This form almost always appears in babies’ legs or feet.
- Early-onset. Primary lymphedema that develops during childhood, adolescence, or early adulthood — especially during periods of rapid growth or hormonal changes — is known as Miege’s disease, or lymphedema praecox.
- Late-onset. Known as lymphedema tarda, this form of primary lymphedema usually affects the legs and is characterized by poor wound healing. This is the least common form of lymphedema, and the triggering event may not be obvious.
Secondary Lymphedema
Secondary lymphedema is more common, and it results from external damage to the lymphatic system. This condition can develop at any age. Swelling usually appears in the arms and legs, but it depends on where the lymphatic system damage occurred. Secondary lymphedema can be triggered by:
- Infections. Severe infections, such as cellulitis, can cause enough damage to the lymph vessels that they are no longer able to function properly, leading to lymphedema.
- Trauma. Injuries, wounds, or surgeries that impact the lymphatic system can lead to secondary lymphedema.
- Inflammatory conditions. Chronic inflammatory diseases like rheumatoid arthritis or chronic venous insufficiency can lead to lymph fluid retention.
- Obesity. Body weight can increase the pressure on the lymphatic system, making it more difficult for lymph fluid to drain properly.
- Tumors. Cancerous tumors can become large enough to put pressure on the lymphatic system, blocking the flow of fluid and leading to buildup in the surrounding tissues.
- Cancer treatments. Radiation therapy or surgical removal of the lymph nodes can damage parts of the lymphatic system, leading to lymphedema.
Lymphedema Symptoms

Symptoms of lymphedema can vary quite a bit, depending on severity, and they may appear gradually or without warning. Common signs of lymphedema include:
- Visible swelling. The most common symptom of lymphedema is swelling, especially in the arms or legs. Swelling may also appear in the face, neck, abdomen, or genitals, depending on the location and cause of the damage.
- A sense of fullness or heaviness in your arms or legs. The fluid buildup can add extra weight to the affected area.
- Arms or legs appear to be different sizes or shapes. The affected limb may look larger, and the size difference can become more noticeable as lymphedema progresses.
- Swelling changes. Depending on your activity levels, diet, and stage of lymphedema, swelling may come and go.
- Reduced range of motion. Swelling can lead to tight, stiff, or inflexible joints, which can make it hard to move as usual.
- Skin changes. Lymphedema can cause the skin to appear puffy, stretched, or red. In some cases, skin can become leathery or thickened.
- Frequent infections. The affected area is at higher risk of infection, especially if the skin is broken. Early signs of infection include redness, warmth, swelling, and fever. Seek medical attention if you suspect an infection.
Lymphedema Causes
Lymphedema can be related to various factors, ranging from the development of the lymphatic system to an injury later in life. Some of the most common causes of lymphedema include:
- Genetic factors. Rarely, people are born with abnormalities in their lymphatic system that lead to primary lymphedema.
- Infections. When the lymphatic system suffers severe or repeated infections, the body is unable to drain fluid, resulting in chronic swelling and inflammation.
- Trauma and surgery. Accidents, surgeries, injuries, or even deep bruises can disrupt the normal flow of lymph fluid.
- Inflammatory conditions. Chronic inflammatory diseases like rheumatoid arthritis or chronic venous insufficiency can lead to lymphedema.
- Parasitic diseases. A certain type of lymphedema, called lymphatic filariasis, is caused by microscopic parasitic worms and spread by mosquito bites.
- Obesity. Lymphedema that is related to excess body weight often appears in the legs.
- Cancer treatments. Surgery or radiation therapy treatments (particularly for breast, pelvic, and prostate cancers) can involve removing or damaging lymph nodes and prevent healthy lymph fluid drainage.
Lymphedema Risk Factors

Most cases of lymphedema are related to external factors like injuries, infections, surgeries, or wounds, which can happen to anyone. However, some people are more at risk than others. Some of the most common risk factors include:
- Age. Lymphedema can occur at any age, but the risk increases with age due to changes in the lymphatic and circulatory systems. Additionally, some age-related conditions like heart disease or kidney disease can increase the likelihood of edema and lymphedema.
- Family history. Primary lymphedema and some lymphatic system disorders tend to run in families.
- Prolonged immobility. Extended periods of low movement, whether due to bed rest or prolonged sitting or standing, can make it difficult for the body to drain lymph fluid as usual.
- Certain medications. Some medications, including NSAIDs, blood pressure medications, corticosteroids, MAOIs, and hormone replacement therapy drugs can have lymphedema as a side effect.
- Underlying health conditions. Conditions that affect fluid balance and circulation can contribute to lymphedema. These conditions can include:
Lymphedema Diagnosis
You may be able to recognize the telltale swelling and skin changes of lymphedema, but only a doctor or healthcare provider can make a diagnosis and provide proper treatment. Diagnosing lymphedema involves a full physical exam and a detailed medical history to determine the cause and severity of the swelling. They will also consider your risk factors, any recent injuries, and your family history.
During the physical examination, the doctor will look for specific signs of lymphedema like:
- Swelling
- Skin changes
- Asymmetrical limbs
- Infections or wounds that won’t heal
Your doctor may recommend additional testing to rule out other conditions that may have similar symptoms. These tests can include:
- MRI or CT scan to view the lymphatic system and surrounding tissues
- Ultrasound to identify where the lymph fluid is accumulating
- Lymphoscintigraphy to visualize the flow of the lymph fluid and identify blockages or abnormalities
Stages of Lymphedema
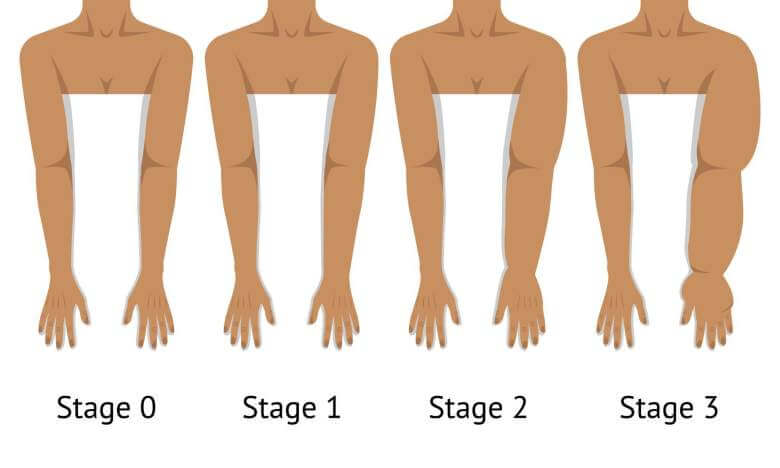
During the diagnosis process, your doctor will determine how severe the swelling is. When left unchecked, lymphedema is a progressive condition that worsens over time, so it’s important to treat or manage symptoms early. According to the International Society of Lymphology, there are four stages of lymphedema:
- Stage zero. No physical signs or symptoms but abnormal lymph fluid flow. This stage is considered sub-clinical, and careful management can slow or even reverse the progression of lymphedema.
- Stage one. Fluid accumulation and swelling that goes away when the area is elevated or compressed. When the swollen area is pressed, it may leave a depression or pit.
- Stage two. Permanent swelling that doesn’t improve with elevation. Stage two lymphedema can also cause skin scarring or thickening. The swollen area is not soft and pressing may not leave a depression.
- Stage three. The most severe form of lymphedema — painful and disfiguring. Medically, stage three lymphedema may be referred to as elephantiasis and is characterized by thickened skin, wart-like growths, and extensive scarring.
Lymphedema Complications
Without treatment, lymphedema can progress and lead to complications that significantly impact quality of life. Some complications include:
- Infections. Lymphedema causes lymph fluid and its contents (including bacteria, wastes, and excess proteins) to build up in the tissues. This increases the risk of skin infections like cellulitis and lymphatic infections like lymphangitis. Both require prompt medical attention.
- Skin changes. Chronic lymphedema can lead to fibrosis, which hardens and thickens the skin. Papillomatosis, which are small wart-like growths, can increase the risk of infection.
- Reduced mobility. Swelling is uncomfortable and can make it hard to do daily tasks, work, exercise, or move swollen joints. In severe cases, lymphedema can lead to permanent disability.
- Circulation complications. Improper compression can impact blood circulation, especially among people with underlying heart conditions like high blood pressure.
- Lymphangiosarcoma. Very rarely, long-term untreated lymphedema can cause this type of soft tissue cancer.
Lymphedema Treatment

There is no cure for lymphedema, but there are several treatments that can help manage symptoms. Managing and treating lymphedema focuses on reducing swelling, preventing complications, and improving quality of life.
- Manual lymphatic drainage. This specialized type of massage helps move lymph fluid out of the swollen areas and into healthy lymph vessels so fluid can flow properly.
- Compression socks and sleeves. Putting even pressure on the parts of the body that are prone to swelling prevents fluid from accumulating.
- Pneumatic compression devices. These specialized devices use air pressure to massage the area and encourage lymph fluid drainage.
- Exercises. Activities like walking, swimming, and cycling can improve lymphatic flow and reduce swelling. A physical therapist can recommend specific activities that promote lymph drainage without putting unnecessary stress on the affected area.
- Elevate legs. When resting, raising swollen legs with pillows or cushions can encourage lymph fluid drainage, especially in the early stages of lymphedema.
- Surgery. In severe cases, surgical options including lymph node transfer or lymphatic bypass may be necessary.
- Medications. Most cases of lymphedema are managed without medications. However, your doctor may prescribe certain drugs to help prevent complications and treat symptoms:
- Antibiotics to treat and prevent infections
- Diuretics (water pills) can help reduce overall swelling
- Benzopyrones may help break down proteins in the lymph fluid and improve flow
- Pain relievers can reduce symptoms and improve movement
Lymphedema Prevention

Although people with primary lymphedema can’t control their genetic factors, there are ways to prevent or slow the progression of lymphedema:
- Skin hygiene. Since lymphedema can cause skin damage and increase the risk of infection, it’s important to take care of the affected skin. Keep the area clean, dry, and moisturized.
- Prevent injuries and care for any wounds. In areas affected by swelling, protect against cuts and scratches to reduce the risk of infection. Treat all injuries promptly — even small cuts, scratches, and bug bites. Tell your doctor about any wounds that don’t heal.
- Wear loose clothing and accessories. Avoid tight socks, pants, jewelry, and rings. Cutting off healthy circulation can lead to excess fluid buildup in your arms, hands, legs, or feet.
- Wear compression garments. Unlike restrictive clothing, compression garments are fitted and apply even pressure that prevents swelling and promotes healthy lymph flow.
- Stay active. Regular physical activity, including gentle stretching, can reduce fluid buildup. At the same time, avoid overexertion and heavy lifting, especially if you are at risk of lymphedema after surgery or when recovering from an injury.
- Manage your weight. Obesity is a significant factor for lymphedema, so achieving and maintaining a healthy weight can reduce the strain on your lymphatic system.
- Healthy lifestyle choices. A balanced diet helps support a healthy weight, and eating well can reduce swelling and promote healing. Follow a nutritious diet that includes plenty of water and limited sodium.
Get the Lowest Price for Lymphedema Medications
If you’re dealing with lymphedema, your doctor might have prescribed medications to help manage the swelling, pain, and any other related conditions. Whatever your treatment includes, you can get the best price for your prescriptions with BidRx.
Place your bid, allow pharmacies to compete for your business, and choose the offer that fits your budget. Depending on the offer, your prescriptions may be available at your local pharmacy or shipped right to your door. Visit our medication page to get started today!
This information is intended for general informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or medication.
