Highlights
- External ulcers are breaks in the skin, occurring either as open sores or in the underlying layers of skin.
- External ulcers are usually caused by a lack of blood flow to an area in the body, for a wide variety of reasons, including chronic illness and staying in the same position for long periods of time.
- Skin ulcers are preventable, and most are treatable.
- Skin ulcers need to be protected from infection.
- Catching ulcers early is the most important way to keep them from becoming more serious.
Skin ulcers, sometimes called skin lesions or sores, are breaks in the skin, either at the surface or underneath. Left untreated, they open the body to infection and other health problems and can keep you from your daily activities. Learn about the different types of external ulcers, why they happen, how they can be treated and prevented, and how to get the support you need for skin ulcers.
Types of External Ulcers
| Type of Ulcer | Common Locations | Appearance | Underlying Causes | Associated Symptoms | Treatment Approaches |
| Venous Ulcer | Lower legs | Shallow, red | Poor venous circulation | Swelling, itching | Compression, wound care |
| Arterial Ulcer | Feet, toes | Deep, pale | Poor arterial circulation | Pain, cold skin | Medications, surgery |
| Diabetic Ulcer | Feet | Callused | Diabetes | Numbness, tingling | Blood sugar control, care |
| Pressure Ulcer | Bony areas | Red, purple | Prolonged pressure | Pain, tenderness | Pressure relief, dressings |
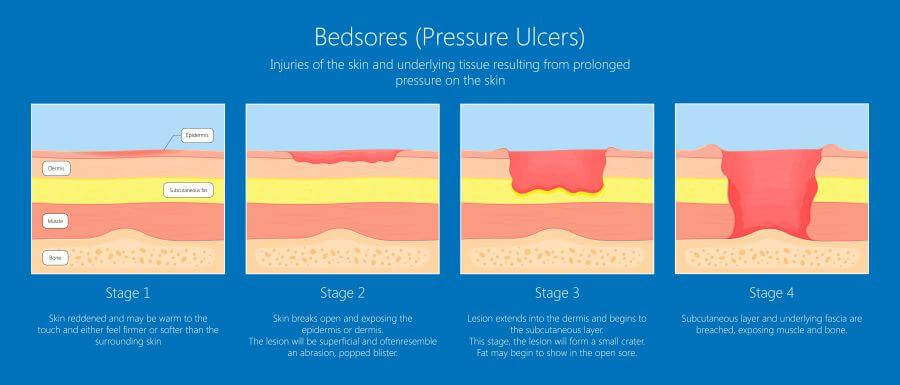
Pressure Ulcers
Pressure ulcers, also known as bedsores or decubitus ulcers, are open sores that occur when pressure is applied to the skin for an extended period of time. This can happen when someone is sitting or lying in the same position for too long, such as when they are bedridden or paralyzed.
Pressure ulcers can occur anywhere on the body, but they are most common on the bony prominences, such as the heels, elbows, hips, and tailbone. This is because these areas have less padding and are more likely to be compressed against a hard surface.
Vascular Ulcers
Vascular ulcers are caused by reduced blood flow to the skin. This can be due to a variety of conditions, including peripheral vascular disease (PVD), chronic venous insufficiency (CVI), and diabetes. Vascular ulcers are most common on the feet and legs, but can also occur on other parts of the body.
Vascular ulcers can be either venous or arterial.
Venous Ulcers
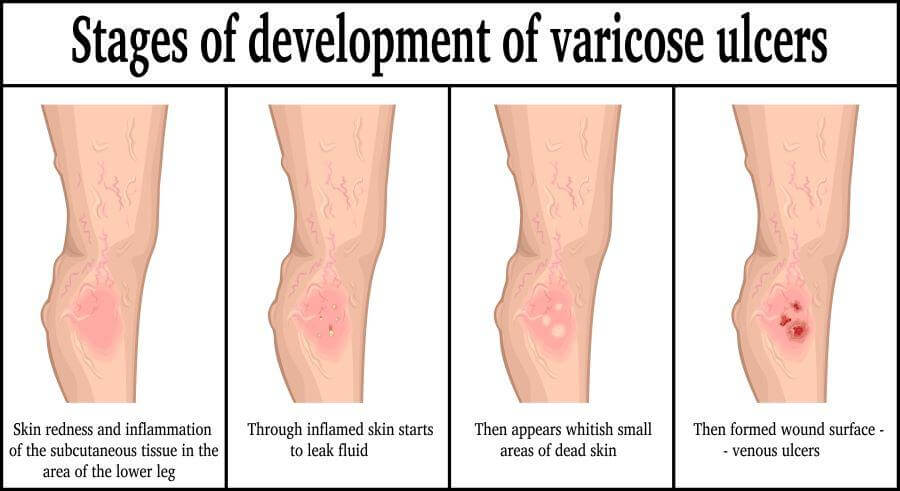
Venous ulcers are a type of vascular ulcer that is caused by CVI. CVI is a condition in which the veins in the legs do not work properly, causing blood to pool in the legs. This pooling of blood can damage the skin and lead to an ulcer. Venous ulcers are most common on the lower legs, near the ankles.
Venous ulcers are often less painful than arterial ulcers, but they can be prone to infection. If not treated right away, venous ulcers can lead to serious complications, such as cellulitis or skin cancer.
Arterial Ulcers
Arterial ulcers are another type of vascular ulcer that is caused by PVD. PVD is a narrowing of the arteries in the legs and feet. This narrowing of the arteries can reduce blood flow to the skin and lead to an ulcer.
Arterial ulcers are often painful and can be difficult to heal. They are also at risk of infection. Like venous ulcers, arterial ulcers must be treated promptly to avoid serious complications, such as amputation.
| Characteristic | Vascular Ulcer | Venous Ulcer | Arterial Ulcer |
| Cause | Reduced blood flow to the skin | Chronic venous efficiency | Peripheral vascular disease |
| Location | Most common on the feet and legs, but can occur anywhere in the body | Most common on the lower legs, near the ankles | Most common on the toes and feet |
| Appearance | Can be shallow or deep, with irregular edges | Often shallow and large, with red or brown skin surrounding the ulcer | Often deep and punched-out, with pale or blue skin surrounding the ulcer |
| Pain | May be painful or painless | May be painful, especially when standing or walking | Often painful, even at rest |
Diabetic Skin Ulcers
People with diabetes are at unique risk for skin ulcers. They are most common on the feet and legs, but can also occur on other parts of the body, such as the hands and buttocks.
Diabetic ulcers can be very painful and difficult to heal. They also have a high risk of infection. If not treated promptly, diabetic ulcers can lead to amputation.
Causes and Risk Factors for Skin Ulcers
You may have noticed a consistent cause for external ulcers — problems with blood circulation. Not everyone with circulatory issues will be at risk for external ulcers, and not everyone with chronic diseases will have the same risk. However, some causes can be treated to reduce risk.
Trauma and Injury
When your body has to heal from accidents or other injuries, it may not restore full blood flow, and in extreme cases, can even completely cut off small areas of the body from blood flow. This is particularly true of the limbs. If you’ve had a severe injury in the past, ask your doctor about blood flow to the area and what can be done if problems arise.
Prolonged Pressure
Pressure ulcers, or bedsores, are caused by a combination of factors, including:
- Pressure: Pressure on the skin reduces blood flow and can damage the tissues.
- Friction: Friction is the force that occurs when two surfaces rub against each other. This can damage the skin and make it more susceptible to infection.
- Shear: Shear is the force that occurs when two surfaces move against each other in opposite directions. This can also damage the tissues.
People who are at risk for developing pressure ulcers include:
- People who are bedridden or paralyzed
- People who have limited mobility
- People with poor circulation
- People with diabetes
- People who are malnourished
- People who are elderly
Diabetes
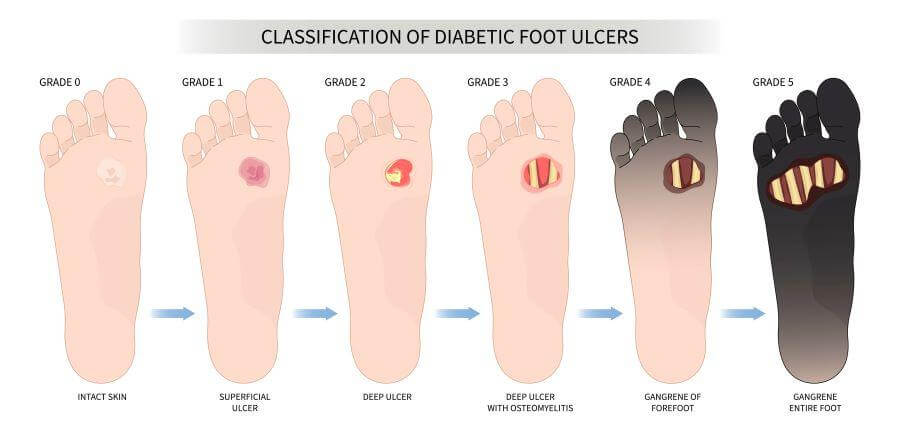
Diabetic ulcers are often the result of a combination of factors such as poor circulation, nerve damage, and high blood sugar levels. Poorly controlled diabetes can lead to inflammation and endothelial dysfunction, which can impair blood flow and contribute to nerve damage.
Diabetic ulcers are most common on the feet and legs, but they can also occur on other parts of the body. They can be very painful and are difficult to heal. If not treated promptly, they can lead to serious infection and even amputation.
Circulatory Disorders and Diseases
Any condition that cuts down on your body’s ability to get blood where it needs to go brings with it a risk of vascular ulcers. This is particularly true of conditions that affect one area of the body, but it can also apply to systemic problems like PVD (arterial ulcers) and CVI (venous ulcers).
While the two types of vascular ulcers are similar, they have different causes.
Vascular Ulcers
While both types of vascular ulcers are caused by circulatory problems, one involves conditions that affect the veins, and the other the arteries.
Venous Ulcers
Venous ulcers are caused by a variety of conditions that impair or obstruct the veins, including:
- Deep vein thrombosis (DVT)
- Varicose veins
- Phlebitis
- Venous insufficiency
- Obesity
- Lack of exercise
- Smoking
Arterial Ulcers
Arterial ulcers are caused by a variety of conditions that narrow or block the arteries, including:
- Atherosclerosis
- Peripheral artery disease (PAD)
- Thromboangiitis obliterans (Buerger’s disease)
- Raynaud’s disease
- Diabetes
- Hypertension
- High cholesterol
- Smoking
Skin Ulcers: Symptoms and Diagnosis
Becoming familiar with the signs of an ulcer can help you distinguish it from other skin problems. Look for:
- Swelling
- Redness
- Tenderness
- Itchiness
- Pain
- Skin discoloration
- Changes in skin texture
Also become familiar with the stages of ulcers, which can help you decide if you need medical attention.
- Stage 1. An uncomfortable or itchy red spot on the skin that doesn’t go away. The outer layer of skin is unbroken.
- Stage 2. The ulcer has broken through the outer layer of skin and is a small wound. There may be some pus or other discharge.
- Stage 3. A larger, deeper wound, possibly with fat tissue visible under the skin. These are particularly serious and need immediate medical attention.
- Stage 4. Muscle or bone may be visible through the skin. Stage 4 ulcers are typically accompanied by signs of serious infection.
Generally, ulcers are diagnosed by a physical examination and a patient history. Depending on the location and your medical history, you may need to undergo a biopsy to rule out other possibilities, such as skin cancer.
External Ulcer Treatment and Management
The most important aspect of treating an ulcer is to keep it clean and away from possible sources of infection. An ulcer can heal quickly and you’ll be at less risk of complications unless it becomes infected, so protection is the mainstay of skin ulcer care.
Wound Care for Skin Ulcers
In many cases, day-to-day treatment will be similar to any other wound. You’ll need to keep the ulcer dry, dress it with sterile bandages, and change the dressing regularly. Depending on the ulcer, antibiotic ointment may be helpful to limit infection.
Medication
Antibiotics are usually prescribed for ulcers with signs of infection. These can be in ointment form or taken orally, depending on the circumstances. Your doctor may recommend over-the-counter medication such as nonsteroidal anti-inflammatory drugs (NSAIDs) to manage the pain. However, they should be used with caution, because NSAIDs can thin the blood, which can increase the risk of bleeding from skin ulcers.
Surgical Treatment
Later-stage ulcers may need debridement, a process where dead tissue is removed from the wound to help it heal. Other types of ulcers may have surgical options as well to treat the underlying causes. Chronic venous insufficiency, for example, can be treated with surgery on the veins to help with blood flow. Some severe ulcers may need skin grafts.
Mental Health and Support
Skin ulcers can be difficult emotionally as well as physically. Both their causes and their symptoms can wear on your mental well-being. Support groups and one-on-one sessions can help you maintain a positive attitude and stay focused on your treatment.
In summary, a number of treatments are available for skin ulcers, depending on the type and severity of the ulcer. Your doctor will work with you to develop a treatment plan that is right for you.
Prevention Strategies

Preventing external ulcers is the best way to maintain your health and catch them early. Take the following steps if you’re at risk of external ulcers.
- Regularly inspect your skin. Look for early signs of ulcers, especially on the feet and hands, and see a doctor if you’re concerned about them.
- Use pressure relief techniques. Even if your mobility is limited, physical therapists and other professionals can teach you how to change your position and redistribute the pressure on your body.
- Maintain a hygiene regimen. While you don’t need antibiotic soap or any special cleaners, make sure to maintain your hygiene regimen even if you need to be immobile for a while.
- Avoid harsh cleaning products. These can irritate the skin and increase the risk of infection.
- Regularly change your position throughout the day. Even staying lightly active will help you maintain your circulation and keep blood from pooling in various places on your body.
- Keep chronic conditions under control as much as possible. Well-controlled chronic conditions are much less likely to result in ulcers.
- Lifestyle changes. Lifestyle changes are an important part of ulcer prevention. Making the following changes can limit your risk and help with management of existing ulcers:
- Quitting smoking
- Regular exercise that encourages circulation
- A vegetable-forward diet
- Physical therapy and training
- Reducing alcohol consumption
You Don’t Have to Live With External Ulcers
Catching potential ulcers early and getting them treated before they become more serious is your best option. Prevention measures are essentially the same as for managing chronic disease and maintaining good overall health. Skin ulcers can be uncomfortable and even frightening, but they’re not inevitable.
Get the Lowest Prices on your Ulcer Medications
Similarly, high drug prices shouldn’t be seen as inevitable. BidRX helps you get the lowest price for your ulcer medication by making it easy to put your prescription up for bid. Pharmacies from around the country will offer you their best price, and you choose the offer that best meets your needs.
See how easy it is to save on all your prescriptions by visiting our medications page to get started!
