Highlights
- NSAIDs are among the most commonly used medications to relieve mild to moderate pain from inflammation associated with conditions like arthritis, headaches, injuries and menstrual cramps.
- They work by blocking enzymes called cyclooxygenase (COX) that participate in the production of inflammatory compounds.
- NSAIDs can help relieve swelling, pain and fever, but may also cause side effects like stomach bleeding and ulcers, kidney problems, ringing in the ears, dizziness and increased heart risks.
- There are two main types of NSAIDs: selective and nonselective.
- NSAIDs interact with several medications, including blood thinners, steroids, diuretics and ACE inhibitors. Use caution when combining NSAIDs with other drugs.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a class of medications widely used for their pain-relieving, fever-reducing, and, as the name suggests, anti-inflammatory properties. Common examples of NSAIDs include aspirin, ibuprofen (Motrin and Advil), and naproxen (Aleve).
NSAIDs are an important part of the treatment of pain, targeting the enzymes that jump-start the process of inflammation. They’re often used to treat conditions like arthritis, menstrual cramps, and various forms of acute pain.
But the devil is in the details. While they’re very effective, NSAIDs can cause a wide range of side effects and drug interactions. This is why it’s important to know the type of NSAID you’re using and the potential benefits and risks of each.
How NSAIDs Work
When an injury or infection occurs in the body, it triggers the release of chemicals that initiate the body’s natural healing response. As part of this process, cyclooxygenase (COX) enzymes are activated. Their job is to produce prostaglandins, which are essential to the healing process but cause inflammation, pain, and fever.
NSAIDs work by blocking the COX enzymes to reduce the amount of prostaglandins they produce.
There are two main COX enzymes:
- COX-1. COX-1 is always active in your body, taking care of everyday functions, like protecting your stomach lining.
- COX-2. COX-2 is a specialist called in for specific tasks, like dealing with pain and inflammation from injuries.
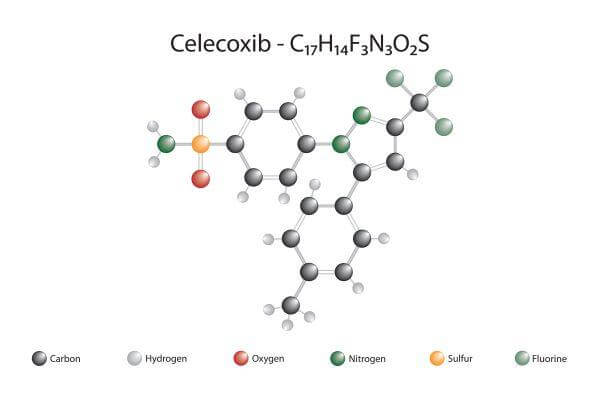
NSAIDs differ in how they affect COX-1 and COX-2. Non-selective (traditional) NSAIDs, like ibuprofen and naproxen, block both, while selective COX-2 inhibitors (like celecoxib) primarily block just COX-2. The challenge is to reduce the prostaglandins that cause pain and inflammation, while trying not to limit the effect on prostaglandins that have protective roles.
The selectivity of NSAIDs can make a difference in the side effects and suitability of an NSAID for different individuals. Here’s a rundown of the types and subtypes of NSAIDs.
Non-Selective (Traditional) NSAIDs
Non-selective NSAIDs work by blocking both the COX-1 and COX-2 enzymes involved in mediating inflammation and pain. Most over-the-counter pain relievers, like ibuprofen (Advil and Motrin) and naproxen (Aleve) are nonselective.
Nonselective NSAIDs can be categorized based on their chemical structure and subtype. Each subtype has its unique characteristics, although they all generally function by inhibiting both COX-1 and COX-2 enzymes.
Here’s an overview of the nonselective NSAID subtypes with examples:
Salicylates
Salicylates are a class of NSAIDs derived from salicylic acid, a compound found naturally in plants.
Examples include:
- Aspirin (acetylsalicylic acid). The first NSAID to be developed, aspirin is still commonly used for inflammation, pain, fever, and to prevent blood clots.
- Diflunisal (Dolobid). Primarily used to relieve pain.
- Methyl salicylate (Ben Gay, IcyHot, Salonpas). Often found in topical pain relief products, such as creams and ointments, used for relieving muscle and joint pain.
- Bismuth salicylate (Pepto Bismol, Kaopectate). Commonly used to treat nausea, heartburn, indigestion, upset stomach, and diarrhea.
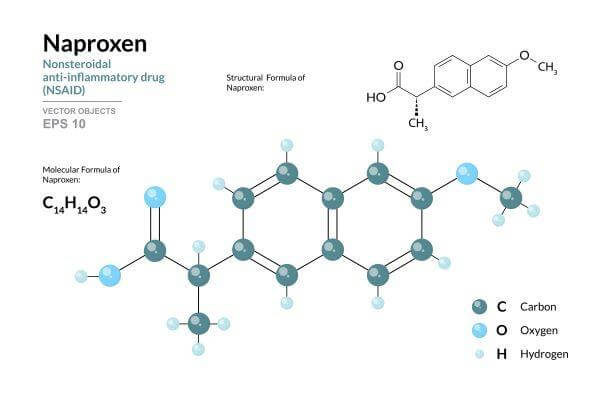
Propionic Acid Derivatives
- Ibuprofen. Widely used for pain, inflammation, and fever.
- Naproxen. Longer acting, used for similar indications as ibuprofen.
- Ketoprofen (Orudis, Oravail). Used for pain, inflammation, and fever.
Acetic Acid Derivatives
- Indomethacin (Indocin, Tivorbex). A potent NSAID often used for treating gout, arthritis, and other inflammatory conditions.
- Diclofenac (Voltaren, Cataflam, Zipsor). Commonly used for arthritis-related inflammatory pains.
- Ketorolac (Toradol). Often used for short-term management of moderate to severe pain, especially following surgery.
- Sulindac (Clinoril). Less commonly used, but effective for certain types of pain and inflammation.
Enolic Acid (Oxicams)
- Piroxicam (Feldene). Used for chronic inflammatory conditions because of its long half-life.
- Meloxicam (Mobic, Vivlodex). Slightly more COX-2 selective but still considered nonselective; used for osteoarthritis and rheumatoid arthritis.
Fenamates
- Mefenamic acid (Ponstel). Often used for short-term pain management, such as for menstrual pain.
- Meclofenamate (Meclomen). Used for various types of arthritis.
While several of these medications are available over the counter, such as aspirin, ibuprofen, naproxen, and diclofenac, most are available by prescription only.
Prescription NSAIDs are used for more severe pain or conditions that over-the-counter NSAIDs may not effectively manage. It’s important to use them under the guidance of a healthcare professional due to the potential for side effects and interactions with other medications.

Warnings and Contraindications — Non-Selective NSAIDs
As non-selective NSAIDs inhibit both COX pathways including the protective COX-1 enzyme, they carry more gastrointestinal, renal, and cardiovascular cautions and contraindications compared to selective NSAIDs.
The specific warnings for non-selective NSAIDs include:
- Gastrointestinal risks: There is an increased risk of developing gastrointestinal ulcers and bleeding with the use of non-selective NSAIDs. This is due to their inhibitory effect on the COX-1 enzyme, which normally helps to protect the lining of the stomach.
- Impaired kidney function. These drugs can impair kidney function. The inhibition of COX enzymes can reduce blood flow to the kidneys, which may lead to kidney damage, especially in individuals with pre-existing renal impairment or those using other drugs that can be toxic to the kidneys.
- Cardiovascular concerns. Prolonged use of non-selective NSAIDs is associated with an increased risk of heart problems and stroke. This risk may be higher in individuals with existing cardiovascular diseases.
- Asthma and aspirin sensitivity. Non-selective NSAIDs are not recommended for use in individuals who are asthmatic or have a known sensitivity to aspirin. These drugs can exacerbate asthma symptoms and may trigger severe allergic reactions in aspirin-sensitive patients.
Side Effects — Non-Selective NSAIDs
Nonselective NSAIDs, which inhibit both COX-1 and COX-2 enzymes, can cause a range of side effects. Here are some of the common ones:
- Stomach pain
- Heartburn
- Nausea
- Gastric ulcers
- Kidney impairment
- Heart attack
- Stroke
- Hypertension (high blood pressure)
- Allergic reactions
- Dizziness
- Headaches
- Liver damage
Drug Interactions — Non-Selective NSAIDs

Potential drug interactions for all nonselective NSAIDs are very similar, though there is some variation among specific drugs in this category. Visit the Drugs.com Drug Interaction Checker for an accurate list of interactions for your specific medication.
The interactions on this list are also very similar to those given above for selective NSAIDs, with a couple of additions.
Here are the most common drug interactions for nonselective (traditional) NSAIDs:
- Anticoagulants. Selective COX-2 inhibitors may increase the risk of bleeding when combined with anticoagulant medications such as warfarin or heparin.
- Aspirin. COX-2 inhibitors can diminish the antiplatelet action of aspirin, increasing the risk of blood clots or stroke.
- Antihypertensive medications. The use of selective COX-2 NSAIDs with any of the following can reduce the effectiveness of the blood pressure medication:
- ACE inhibitors like lisinopril
- Beta blockers, like metoprolol
- Angiotensin II receptor blockers (ARBs), like losartan
- Diuretics. Taking these NSAIDs with thiazide diuretics, such as furosemide, or loop diuretics, like hydrochlorothiazide, can reduce the effectiveness of the diuretic.
- Selective serotonin reuptake inhibitors (SSRIs). Taking SSRIs, such as fluoxetine or sertraline, with COX-2 inhibitors can increase the risk of GI bleeding.
- Lithium. COX-2 inhibitors can cause increased lithium levels in the blood, which can lead to toxicity.
- Methotrexate. COX-2 inhibitors can cause increased methotrexate levels in the blood, which can lead to toxicity.
- Corticosteroids. When combined with COX-2 inhibitors, corticosteroids like prednisone can cause GI bleeding or ulcers.
- Cyclosporine and tacrolimus. Taking selective COX-2 NSAIDs together with the immunosuppressants cyclosporine or tacrolimus carries an increased chance of kidney toxicity.
- Other NSAIDs. NSAIDs taken with other NSAIDs can cause an increased risk of side effects.
- Digoxin. When used concurrently, selective COX-2 NSAIDs can impair digoxin clearance leading to increased blood levels of the drug.
- Antacids. Antacids containing aluminum or magnesium hydroxide can reduce the body’s absorption of NSAIDs, reducing their effectiveness.
- Proton pump inhibitors (PPIs). PPIs, like omeprazole, can increase the risk of kidney damage when combined with NSAIDs.
- Bisphosphonates. Taking bisphosphonates, like alendronate, with NSAIDs can increase the risk of stomach irritation.
When you’re taking NSAIDs, be sure all of your providers know about all the medications, supplements, and herbal remedies you’re taking. Also, if you have any new or unusual symptoms after beginning a new medication, report them to your doctor right away.
Selective NSAIDS (COX-2 Inhibitors)
Selective COX-2-inhibitors target only the COX-2 enzyme pathway responsible for inflammation and pain. They don’t block the protective COX-1 enzyme, meaning they tend to have fewer gastrointestinal side effects than the nonselective, or traditional, NSAIDs.
COX-2 inhibitors are often used for conditions where inflammation is a significant component, such as arthritis, gout, and musculoskeletal injuries.
Examples of COX-2 inhibitors are celecoxib (Celebrex) and meloxicam.
Warnings and Contraindications — Selective COX-2 Inhibitors
Drugs in this subtype carry the following warnings:
- Increased risk of heart attack and stroke
- Allergic reactions
- Abnormal liver enzyme tests
Side Effects — Selective COX-2 Inhibitors
The most common side effects of selective COX-2 inhibitors include:
- Skin rashes
- Headaches
- Abdominal pain
- Edema (Swelling)
- Hypertension
- Respiratory infections
Drug Interactions — Selective COX-2 Inhibitors
COX-2 NSAIDs can potentially interact with other medications, especially those related to bleeding, blood pressure, kidney function and certain immunosuppressants.
Here are most common drug interactions for selective COX-2 inhibitors:
- Anticoagulants. Selective COX-2 inhibitors may increase the risk of bleeding when combined with anticoagulant medications such as warfarin or heparin.
- Aspirin. COX-2 inhibitors can diminish the antiplatelet action of aspirin, increasing the risk of blood clots or stroke.
- Antihypertensive medications. The use of selective COX-2 NSAIDs with any of the following can reduce the effectiveness of the blood pressure medication:
- ACE inhibitors like lisinopril
- Beta blockers, like metoprolol
- Angiotensin II receptor blockers (ARBs), like losartan
- Diuretics. Taking these NSAIDs with thiazide diuretics, such as furosemide, or loop diuretics, like hydrochlorothiazide, can reduce the effectiveness of the diuretic.
- Selective serotonin reuptake inhibitors (SSRIs). Taking SSRIs, such as fluoxetine or sertraline, with COX-2 inhibitors can increase the risk of GI bleeding.
- Lithium. COX-2 inhibitors can cause increased lithium levels in the blood, which can lead to toxicity.
- Methotrexate. COX-2 inhibitors can cause increased methotrexate levels in the blood, which can lead to toxicity.
- Corticosteroids. When combined with COX-2 inhibitors, corticosteroids like prednisone can cause GI bleeding or ulcers.
- Cyclosporine and tacrolimus. Taking selective COX-2 NSAIDs together with the immunosuppressants cyclosporine or tacrolimus carries an increased chance of kidney toxicity.
- Other NSAIDs. NSAIDs taken with other NSAIDs can cause an increased risk of side effects.
- Digoxin. When used concurrently, selective COX-2 NSAIDs can impair digoxin clearance leading to increased blood levels of the drug.
- Antacids. Antacids containing aluminum or magnesium hydroxide can reduce the body’s absorption of NSAIDs, reducing their effectiveness.
No list of potential drug interactions is complete, and the degree and effects of these medications can vary with the specific NSAID you’re taking. To get a list of potential interactions for a specific medication, visit the Drugs.com Drug Interaction Checker.
A Final Word

NSAIDs are real lifesavers when it comes to knocking out pain and inflammation. They’re great for everything from arthritis to headaches, but these drugs can be a double-edged sword: They do a great job at easing pain and reducing fever, but they can cause some not-so-great side effects, especially if you’re taking them often or mixing them with other meds.
The key is knowing what you’re dealing with and keeping your doctor informed about all medications you’re taking and your medical history. They will help you decide which of the many NSAID options offers the best benefit-to-risk ratio for your situation.
Get the Lowest Price for Your NSAIDs
Now that you’ve educated yourself about NSAIDs, check out BidRx for the lowest price for your medication. Create a bid, and pharmacies will bid on your prescription, allowing you to choose your offer. Create a bid today and start getting the lowest price for your NSAID medications.