Highlights
- Antidepressants are common prescription medications used to treat depression.
- There are several types of antidepressants, including SSRIs, SNRIs, TCAs, DNRIs, MAOIs, NaSSAs, SARIs, and atypical antidepressants.
- Antidepressants work by targeting neurotransmitters in the brain and increasing their availability, leading to an uplift in mood.
- All antidepressants carry an increased risk of developing suicidal thoughts and behaviors in children, teens, and young adults.
- Antidepressants are generally safe for most individuals, but certain individuals (such as those with a history of seizures or angle-closure glaucoma) may need to take antidepressants with caution or avoid them altogether.
- This information is not a substitute for professional medical advice and should be used as a reference guide only.
Depression is a serious condition that can affect every aspect of daily life. Without treatment, depression can often worsen over time and impact emotional and behavioral health. While there is no cure for depression, prescription medications can improve the symptoms and lead to a happier, healthier, more productive life.
This guide to antidepressants shares key information about prescription antidepressants so you can make an informed decision for your health.
What Are Antidepressants?
Antidepressants are a type of medication used to treat depression and other mental health disorders. These medications work by regulating neurotransmitters in the brain, which affect mood and emotions. Antidepressants are available by prescription only and are taken under the guidance of a healthcare professional.

It’s estimated that 11% of Americans age 12 and older take antidepressants.
How Do Antidepressants Work?
Contrary to popular belief, antidepressants don’t simply make a person happy or numb their emotions; instead, they work by regulating neurotransmitters in the brain such as serotonin and norepinephrine. These chemicals play a crucial role in mood regulation, and by adjusting their levels, antidepressants can help alleviate symptoms of depression.
The precise mechanism of action can vary by antidepressant. For example, selective serotonin reuptake inhibitors (SSRIs) specifically target serotonin levels in the brain. The medication prevents neurotransmitters from reabsorbing the serotonin receptors, which makes more serotonin available in the brain.
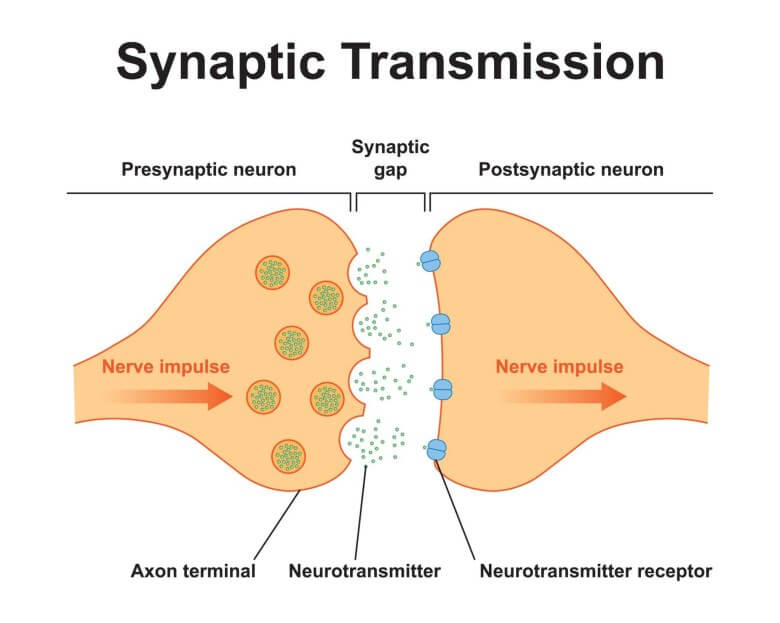
Other antidepressants have a similar mechanism of action, based on the type of neurotransmitter they target.
Finding the right antidepressant can be a trial-and-error process due to how different people respond to different antidepressants. Some antidepressants may also have more side effects than others.
| Type of Antidepressant | Description | Examples |
| Selective serotonin reuptake inhibitors (SSRIs) | Increase serotonin levels in the brain by blocking its reabsorption | fluoxetine (Prozac)
sertraline (Zoloft) citalopram (Celexa) |
| Serotonin-norepinephrine reuptake inhibitors (SNRIs) | Work similarly to SSRIs but target two neurotransmitters: serotonin and norepinephrine | venlafaxine (Effexor)
duloxetine (Cymbalta) desvenlafaxine (Pristiq) |
| Tricyclic antidepressants (TCAs) | Affect multiple neurotransmitters, including serotonin and norepinephrine | amitriptyline (Elavil) nortriptyline (Pamelor)
imipramine (Tofranil) |
| Monoamine oxidase inhibitors (MAOIs) | Inhibit the activity of monoamine oxidase, an enzyme that breaks down neurotransmitters like serotonin, dopamine, and norepinephrine in the brain | phenelzine (Nardil)
tranylcypromine (Parnate) |
| Noradrenergic and specific serotonergic antidepressant (NaSSAs) | Increase noradrenaline and serotonin in the brain while blocking certain serotonin receptors | mirtazapine (Remeron)
mianserin (Tolvon) |
| Serotonin antagonist and reuptake inhibitors (SARIs) | Block serotonin receptors and prevent the reuptake of serotonin. | trazodone (Desyrel)
nefazodone (Serzone) |
| Atypical antidepressants | Don’t fit neatly into other categories | bupropion (Wellbutrin, Zyban)
mirtazapine (Remeron) |
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective serotonin reuptake inhibitors are the most prescribed type of antidepressant. They work by increasing serotonin levels in the brain. Serotonin regulates mood, and SSRIs block its reabsorption to increase its availability.

Examples of SSRIs include:
- Fluoxetine (Prozac)
- Sertraline (Zoloft)
- Citalopram (Celexa)
Warnings and Contraindications — SSRIs
In general, SSRIs have been known to increase suicidal thoughts in children and teens. It’s also believed that SSRIs could impact brain development in individuals under the age of 18.
Some SSRIs may cause blurred vision, drowsiness, or dizziness, so don’t drive a car or operate potentially dangerous machinery until you know how your medication will affect you.
SSRIs may not be suitable for individuals with the following conditions:
- Bipolar disorder
- Epilepsy
- Narrow-angle glaucoma
- Kidney problems
- Liver problems
- Heart problems
- Type 1 or type 2 diabetes
- Bleeding disorders
- Pregnancy or plans to become pregnant
There’s also a risk of developing serotonin syndrome, a serious and potentially life-threatening condition that develops from excess serotonin.
Check with your provider about your specific medication and medical history to be sure an SSRI is the right choice for you.
Side Effects — SSRIs
Side effects can vary by medication, and not everyone experiences side effects. In general, SSRIs can cause the following adverse effects:
Common Side Effects
- Nausea, headache, dizziness
- Dry mouth, sweating, diarrhea, constipation, fatigue
- Sexual dysfunction (decreased libido, orgasm issues)
- Anxiety, agitation, nervousness
- Weight changes (gain or loss)
Less Common Side Effects
- Rash, blurred vision, tremor
- Difficulty urinating
- Increased energy/restlessness
- Decreased appetite
- Sleep disturbances (hyper- or hyposomnia)
- Balance problems
- Muscle twitches
Serious Side Effects
Seek immediate medical attention if you experience signs of any of the following:
- Serotonin syndrome: High fever, confusion, muscle rigidity, seizures
- Mania: Increased energy, racing thoughts, impulsivity
- Suicidal thoughts or behavior: Increased thoughts of self-harm or suicide plans
- Allergic reactions: Skin rash, hives, swelling, breathing difficulties
- Severe bleeding: Easy bruising, nosebleeds, blood in stool
- Irregular heartbeat: Racing heart, skipping beats, chest pain
When taking SSRIs, side effects are often part of the adjustment process and usually go away within a few days. However, severity and specific side effects can vary between individuals and different SSRIs, so always report any concerning side effects to your doctor.
Drug Interactions — SSRIs
SSRIs could potentially interact with other drugs and supplements. Following is a general list of interactions associated with SSRIs. Not all of these interactions apply to all SSRIs, so it’s important to talk to your doctor about your specific situation.
Increased serotonin levels:
- Serotonin syndrome: Combining SSRIs with other drugs that boost serotonin (e.g., triptans, MAOIs, St. John’s wort) can lead to this potentially serious condition with symptoms like agitation, fever, tremor, and confusion.
- Increased bleeding risk: Combining SSRIs with NSAIDs (e.g., ibuprofen, aspirin) or antiplatelets (e.g., clopidogrel) can increase bleeding risk.
Changes in drug metabolism:
- Elevated drug levels: SSRIs can inhibit the breakdown of other medications, leading to higher levels and increased side effects. This can occur with some antipsychotics, tricyclic antidepressants, and medications like metoprolol.
- Reduced drug levels: Conversely, SSRIs can induce the breakdown of some medications, lowering their effectiveness. This can occur with tamoxifen (breast cancer treatment) and warfarin (blood thinner).
Other potential interactions:
- Lithium: SSRIs can increase lithium levels, requiring careful monitoring.
- Seizure risk: Combining SSRIs with medications that lower the seizure threshold (e.g., tramadol) may increase seizure risk.
- General central nervous system (CNS) depression: Combining SSRIs with other CNS depressants (e.g., alcohol, benzodiazepines) can increase drowsiness and sedation.
Refer to the Drugs.com Drug Interaction Checker for your specific medication for a complete list of potential interactions. This is not an exhaustive list, and specific interactions will vary depending on the SSRI and other medications you may be taking.
Always consult your doctor or pharmacist before taking any new medication while on SSRIs. They can assess potential interactions and advise on safe use.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Serotonin-norepinephrine reuptake inhibitors work similarly to SSRIs but target two neurotransmitters: serotonin and norepinephrine. Because they focus on two neurotransmitters, SNRIs may be effective in treating a wider range of depression and anxiety symptoms.

Examples of SNRIs include:
- Venlafaxine (Effexor)
- Duloxetine (Cymbalta)
- Desvenlafaxine (Pristiq)
Warnings and Contraindications — SNRIs
SNRIs carry similar warnings and contraindications to SSRIs. These warnings can also vary by medication. For example:
- Venlafaxine and desvenlafaxine may increase your blood pressure.
- Duloxetine could worsen liver problems.
- Levomilnacipran can increase the risk of abnormal bleeding.
SNRIs have also been shown to increase the risk of suicidal thoughts in children and teens.
Serotonin syndrome has also been reported with SNRIs, both when taken alone or along with other serotonergic medications.
SNRIs aren’t generally recommended to pregnant women unless the benefits clearly outweigh the risks to the mother and baby. These medications may pass into breast milk, so let your doctor know if you are currently breastfeeding or plan to breastfeed.
Ask your doctor for a complete list of warnings and contraindications for your medication.
Side Effects — SNRIs
SNRIs may cause side effects, many of which resolve after taking the medication for several days. These side effects may include but are not limited to:
- Drowsiness
- Muscle weakness
- Agitation
- Dizziness
- Sleep trouble
- Dry mouth
- Constipation
- Increased heart rate
- Headache
- Nausea
- Changes in appetite
These side effects may affect individuals differently, and not all individuals will experience adverse effects. Speak with your doctor if you have any concerns.
Drug Interactions — SNRIs
SNRIs may interact with other drugs. These interactions can vary by medication. Speak to your prescriber about potential interactions to be aware of relative to your personal medical history.
Following is a general list of potential interactions for SNRIs:
Serious Risk (avoid with these medications)
- MAOI antidepressants: Avoid these completely. Combining them with SNRIs can trigger a life-threatening condition called serotonin syndrome.
- TCA antidepressants: Mixing these with SNRIs can also increase the risk of serotonin syndrome and other serious side effects.
- Other SNRI antidepressants: May increase the risk of developing serotonin syndrome.
Moderate Risk (use with caution)
- Triptans (migraine meds): Combining them with SNRIs can raise blood pressure and risk serotonin syndrome. Talk to your doctor about dosage adjustments.
- Anticoagulants (blood thinners): SNRIs can increase their effects, raising the risk of bleeding. Close monitoring is needed.
- Antihistamines: Some types (sedating ones) can increase drowsiness and dizziness when taken with SNRIs. Consider non-drowsy antihistamines instead.
- Alcohol: Can worsen depression and amplify SNRIs’ side effects like dizziness and drowsiness. Best to avoid.
- Other medications: SNRIs can interact with various other drugs, potentially affecting their effectiveness or side effects. Always tell your doctor about all medications and supplements you’re taking.
- Antipsychotics (droperidol, haloperidol): May increase the level of the antipsychotic medication in the blood, which may lead to heightened side effects.
- Antimalarials (such as hydroxychloroquine): May increase the risk of an irregular heartbeat, which can be life-threatening.
- Anxiolytics (such as buspirone): May increase the risk of developing serotonin syndrome.
This isn’t an exhaustive list of potential interactions. Use the Drugs.com Drug Interaction Checker to learn more about your specific SNRI medication. And be sure to notify your provider right away if you experience new or unusual symptoms after beginning an SNRI.
Tricyclic Antidepressants
An older class of medications compared to SSRIs and SNRIs, tricyclic antidepressants affect multiple neurotransmitters, including serotonin and norepinephrine. They have a different chemical structure and mechanism of action and are known for causing more side effects compared to newer antidepressants.

Examples of tricyclic antidepressants include:
- Amitriptyline (Elavil)
- Nortriptyline (Pamelor)
- Imipramine (Tofranil)
Warnings and Contraindications — Tricyclic Antidepressants
Tricyclic antidepressants carry similar warnings as other subtypes of antidepressants, including the risk of developing serotonin syndrome and an increased risk of suicidal thoughts or behaviors.
Individuals with the following conditions should avoid taking TCAs or take these medications with caution:
- Bipolar disorder
- History of seizures
- Cardiovascular disorders
- Hyperthyroidism
- Pregnancy or breastfeeding
TCAs should not be taken with other TCAs, MAOIs, SNRIs, SSRIs, and other antidepressants.
Speak with your doctor about concerns with your specific medication.
Side Effects — Tricyclic Antidepressants
Tricyclic antidepressants may cause side effects similar to those of SSRIs or SNRIs. However, TCAs are prescribed less often than other forms of antidepressants because they are associated with more adverse side effects.
These include:
- Disorientation
- Confusion
- Heart rhythm problems
- More frequent seizures in individuals who have seizures
Be sure to read the patient guide that comes with your prescription to learn about potential side effects.
Drug Interactions — Tricyclic Antidepressants
Drug interactions with tricyclic antidepressants can vary by medication. Following is a list of potential interactions to be aware of TCAs in general:
Risk of Serious Interactions (avoid combining with these medications):
- MAOIs: Can cause a life-threatening “serotonin syndrome” with high fever, confusion, seizures, and muscle rigidity.
- Epinephrine (EpiPen): Can significantly increase blood pressure and heart rate.
- Linezolid (Zyvox): Can also cause serotonin syndrome.
- Tramadol (Ultram): Increases risk of serotonin syndrome.
High Risk (caution needed)
- SSRIs: Increased risk of serotonin syndrome, especially with higher doses. Examples include fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft).
- Anti-arrhythmic drugs (e.g., quinidine, procainamide): Can increase risk of heart rhythm problems.
- Cimetidine (Tagamet): Raises TCA levels in the body, increasing side effects.
- Bupropion (Wellbutrin): May increase risk of seizures.
- Lithium: Potential for toxicity and altered blood levels of both medications.
Moderate Risk (monitor for interactions)
- Alcohol: Can worsen drowsiness and sedation caused by TCAs.
- Barbiturates and other sedatives: Increased risk of drowsiness and respiratory depression.
- Antipsychotics: May increase risk of side effects like tardive dyskinesia.
- Anticholinergics (e.g., scopolamine): Additive effects on dry mouth, constipation, and urinary retention.
- Decongestants and asthma medications: May raise blood pressure and heart rate.
This is not an exhaustive list. Consult your doctor or pharmacist for a complete picture of potential interactions, or visit the Drugs.com Drug Interaction Checker.
Always disclose all medications, supplements, and herbs you are taking when starting or changing a TCA medication. Your doctor may need to adjust dosages or choose alternative medications if potential interactions are a concern.
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine oxidase inhibitors (MAOIs) are among the first antidepressants developed. They inhibit the activity of monoamine oxidase, an enzyme that breaks down neurotransmitters like serotonin, dopamine, and norepinephrine in the brain.
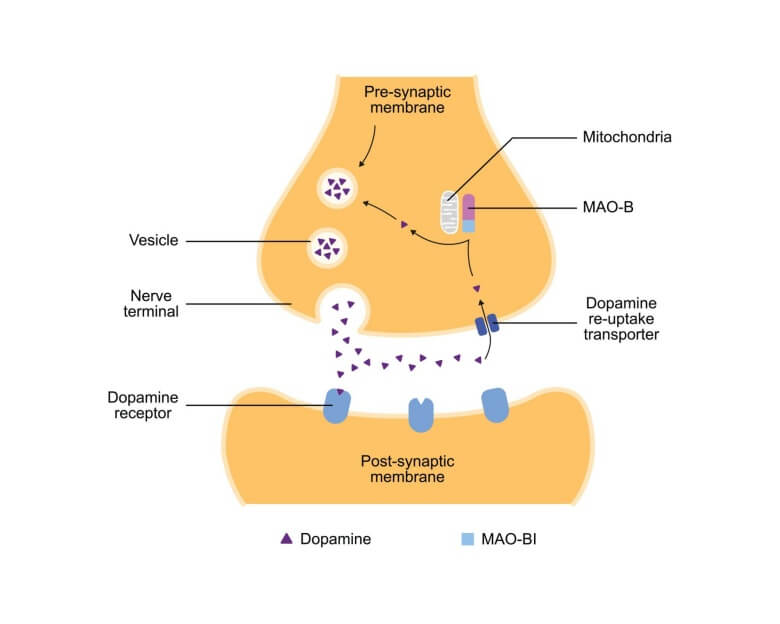
MAOIs are not a first-line choice for treating depression, but they have been shown to be effective in treating atypical depression in individuals who don’t respond well to other classes of antidepressants.
However, MAOIs may also carry more potential side effects and dietary restrictions due to their interaction with certain foods and other medications.
Examples of MAOIs include:
- Phenelzine (Nardil)
- Tranylcypromine (Parnate)
- Isocarboxazid (Marplan)
Warnings and Contraindications — MAOIs
Research suggests the following individuals should not receive MAOI therapy:
- History of alcoholism
- Angina
- Diabetes
- Kidney disease
- Blood vessel disease
- A recent heart attack or stroke
- Liver disease
- Overactive thyroid
- Pheochromocytoma (vascular tumor of the adrenal medulla)
Additional warnings and contraindications may vary by medication. For example, the medication phenelzine also lists congestive heart failure and abnormal liver function under its contraindications.
MAOIs should not be taken in conjunction with other antidepressants.
These medications may also impact the breakdown of tyramine, which is found in certain foods, drinks, and medications. A high level of tyramine in the body may suddenly increase blood pressure or lead to a cerebral hemorrhage, which can result in death.
MAOIs may also increase the risk of suicidal thinking and behavior in adolescents and young adults who have been diagnosed with MDD and other psychiatric disorders. Anyone considering an MAOI must balance these risks with clinical needs.
Side Effects — MAOIs
MAOIs are not the first choice for treating mental health disorders because of the side effects and other concerns. However, they have proven effective for individuals who haven’t responded well to other treatments.
The following side effects may occur when taking an MAOI:
- Dry mouth
- Nausea
- Diarrhea
- Insomnia
- Drowsiness
- Dizziness
- Constipation
- Lightheadedness
Other serious side effects have occurred. These may include but are not limited to:
- Fever
- Confusion
- Muscle stiffness
- Seizures
- Liver or kidney problems
Talk to your doctor about any new or worsening side effects or if you have any concerns when taking this medication.
Drug Interactions — MAOIs
Potential drug interactions may vary among medications, so speak to your doctor about your specific prescription or visit the Drugs.com Drug Interaction Checker to learn more.
Following is a general guide to known drug interactions with MAOIs:
Risk of Serotonin Syndrome
High risk:
- SSRIs: fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), etc.
- SNRIs: Venlafaxine (Effexor), duloxetine (Cymbalta), etc.
- TCAs: Clomipramine (Anafranil), imipramine (Tofranil), etc.
- Some pain relievers: Meperidine (Demerol), fentanyl, tramadol (Ultram), etc.
- Certain herbal supplements: St. John’s wort, tryptophan, ginseng, etc.
Moderate risk:
- Lithium: Monitor for toxicity and altered blood levels.
- Buspirone (Buspar): Increased risk of serotonin syndrome, especially with higher doses.
Risk of Hypertensive Crisis
- Direct-acting sympathomimetics: Decongestants (pseudoephedrine, phenylephrine), diet pills, amphetamines, cocaine.
- Indirect-acting sympathomimetics: Ephedrine, methamphetamine, some nasal sprays.
Other Potential Interactions
- Barbiturates and benzodiazepines: Increased drowsiness and respiratory depression.
- Opioids: Additive sedation and respiratory depression.
- Antipsychotics: Increased risk of side effects like tardive dyskinesia.
- Anticholinergics: Worsening of dry mouth, constipation, and urinary retention.
- Alcohol: Increased drowsiness and sedation.
For a complete list of interactions, refer to the Drug Interaction Checker for your specific medication.
Noradrenergic and Specific Serotonergic Antidepressants (NaSSAs)
Noradrenergic and specific serotonergic antidepressants (NaSSAs) increase noradrenaline and serotonin in the brain while blocking certain serotonin receptors.

The only NaSSA commonly prescribed in the U.S. is mirtazapine, which is used to treat depression, anxiety, and insomnia. Brand names include Remeron, Avanza, and Zispin.
Warnings and Contraindications — NaSSAs
As with other types of antidepressants, warnings and contraindications may vary by medication.
Mirtazapine should not be taken at the same time as an MAOI or within 14 days of discontinuation of an MAOI. Doing so may lead to the development of serotonin syndrome.
Some patients may experience worsening of their depression when starting mirtazapine. This may lead to an increase in suicidal thinking and behaviors.
All antidepressants, including NaSSAs, carry a warning of the potential for suicidal thinking and behavior in children, teens, and young adults.
Check your medication’s insert for a complete list of warnings and contraindications.
Side Effects — NaSSAs
Side effects of NaSSAs may include but are not limited to:
- Dry mouth
- Increased appetite
- Constipation
- Weight gain
- Dizziness
- Drowsiness
- Trouble sleeping
Contact your doctor right away if you experience any of the following side effects:
- Suicidal thoughts
- Suicide attempts
- Worsening depression or anxiety
- Panic attacks
- Feelings of aggression
- Unusual changes in mood or behavior
For more information regarding possible side effects, consult with your doctor.
Drug Interactions — NaSSAs
Like most drugs, mirtazapine has a known potential for interactions with other medications. Here are the major interactions to be aware of:
Serious Risk (avoid combining with):
- Monoamine oxidase inhibitors (MAOIs): Can cause a life-threatening condition called serotonin syndrome with symptoms like fever, confusion, seizures, and muscle rigidity.
- Linezolid (Zyvox): Also increases risk of serotonin syndrome.
Hgh Risk (use with caution):
- SSRIs: Increased risk of serotonin syndrome, especially with higher doses. Examples include fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft).
- TCAs: Can potentially trigger serotonin syndrome or worsen mirtazapine’s side effects.
- Lithium: May increase risk of toxicity and require dosage adjustments.
- Cyclobenzaprine (Flexeril): Both increase serotonin levels, raising the risk of serotonin syndrome.
- Clonidine (Catapres): Mirtazapine can counteract its blood pressure-lowering effects.
- Guanethidine (Ismelin): Similar to clonidine, mirtazapine can reduce its effectiveness.
Moderate risk (monitor for interactions):
- Benzodiazepines (Xanax, Valium): Can worsen drowsiness and sedation caused by mirtazapine.
- Barbiturates (Luminal, Seconal): Same as benzodiazepines, increased risk of drowsiness and respiratory depression.
- Warfarin (Coumadin): May increase the risk of bleeding when taken with mirtazapine.
- Carbamazepine (Tegretol): Can lower mirtazapine levels, reducing its effectiveness.
- St. John’s wort: Similar to SSRIs, can potentiate serotonin syndrome.
Many other medications may interact with mirtazapine, so speak with your provider or refer to the Drugs.com Drug Interaction Checker for a complete list of known interactions.
Serotonin Antagonists and Reuptake Inhibitors (SARIs)
Serotonin antagonists and reuptake inhibitors (SARIs) block serotonin receptors and prevent the reuptake of serotonin.
These medications fall under the antidepressant umbrella but are more commonly used to treat other conditions, such as anxiety and insomnia.

Trazodone is the most commonly used SARI in the U.S. It is also available as the following brand names:
- Desyrel Dividose
- Oleptro
- Trazodone D
Nefazodone (Serzone) is another SARI that is still used but less commonly due to liver side effects.
Warnings and Contraindications — SARIs
SARIs should not be taken with other antidepressants, as this may increase the risk of developing serotonin syndrome.
Patients with narrow-angle glaucoma should not take SARIs or other antidepressants.
Other warnings and contraindications may vary by medication. For example, trazodone carries the following warnings:
- Increased risk of bleeding if also taking aspirin, NSAIDs, warfarin, or other antiplatelet drugs
- Priapism may occur, which requires immediate medical attention
- Possible activation of mania or hypomania
- Potential for motor and cognitive impairment
- Increased risk of developing orthostatic hypotension and syncope
Trazodone increases the QT interval. Patients should avoid taking other drugs that increase the QT interval or have risk factors for a prolonged QT interval.
Side Effects — SARIs
Trazodone and nefazodone have similar side effects, though trazodone is a little less potent as an antidepressant. However, it tends to be more sedating than nefazodone, so it’s less suitable for daytime use.
Nefazodone has the additional side effect of liver toxicity, so liver function monitoring is usually recommended for users of this medication.
Common side effects of SARIs include:
- Dry mouth
- Blurred vision
- Headache
- Dizziness
- Drowsiness
- Fatigue
Individuals who suddenly stop taking this medication may experience withdrawal symptoms.
Contact your doctor if you experience less common but serious side effects, including:
- An erection lasting longer than six hours (priapism)
- Blood pressure drops when standing up from a seated position
- Fainting
- Irregular or fast heartbeat
- Unusual bleeding or bruising
- Sexual dysfunction
- Constipation
- Insomnia
- Agitation
- Tremor
- Confusion
- Weight changes
- Rash
Speak with your doctor about all the possible side effects of your specific medication.
Drug Interactions — SARIs
Examples of major drug interactions with trazodone include but are not limited to:
Serotonin Syndrome
High risk:
- SSRIs: Fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), etc.
- SNRIs: Venlafaxine (Effexor), duloxetine (Cymbalta), etc.
- TCAs: Clomipramine (Anafranil), imipramine (Tofranil), etc.
- Some pain relievers: Meperidine (Demerol), fentanyl, tramadol (Ultram), etc.
- Certain herbal supplements: St. John’s wort, tryptophan, ginseng, etc.
Moderate risk:
- Lithium: Monitor for toxicity and altered blood levels.
- Buspirone (Buspar): Increased risk of serotonin syndrome, especially with higher doses.
Hypertensive Crisis
- Direct-acting sympathomimetics: Decongestants (pseudoephedrine, phenylephrine), diet pills, amphetamines, cocaine.
- Indirect-acting sympathomimetics: Ephedrine, methamphetamine, some nasal sprays.
Other Potential Interactions
- Barbiturates and benzodiazepines: Increased drowsiness and sedation.
- Opioids: Additive sedation and respiratory depression.
- Antipsychotics: Increased risk of side effects like tardive dyskinesia.
- Anticholinergics: Worsening of dry mouth, constipation, and urinary retention.
- Arsenic trioxide (a medication that slows the growth of cancer cells): May increase the risk of developing an irregular heartbeat, which could be serious and life-threatening.
- Cabozantinib (a cancer treatment to slow or stop the spread of cancer cells): May increase the risk of developing an irregular heart rhythm.
- Fingolimod (a medication that decreases the activity of immune cells): Could develop an irregular heartbeat, which is most likely to occur within the first 20 hours of taking your first dose.
- Alcohol
Visit the Drugs.com Drug Interaction Checker for the complete list regarding your medication.
Atypical Antidepressants
This category includes antidepressants that don’t fit neatly into the other categories. They may target different neurotransmitters or have unique mechanisms of action.
They might also have additional use cases, such as bupropion as a smoking cessation drug.

Bupropion (Wellbutrin, ZYBAN) is an example of an atypical antidepressant.
Warnings and Contraindications — Atypical Antidepressants
Because these antidepressants don’t fit neatly into other categories, it’s essential to consider each one’s unique warnings and contraindications.
Keep in mind all antidepressants, including atypical ones, carry a risk of increased suicidal thoughts and behaviors in children, teens, and young adults.
Check your specific medication’s label for warnings and contraindications, or better still, talk to your prescriber.
Side Effects — Atypical Antidepressants
Side effects may vary among atypical antidepressants.
Potential side effects of bupropion may include:
- Dry mouth
- Sore throat
- Stuffy nose
- Blurred vision
- Nausea
- Vomiting
- Headache
- Dizziness
- Weight loss
- Loss of appetite
- Constipation
- Sleep trouble
Serious side effects may also occur, including:
- Allergic reactions
- Seizures
- Manic episodes
- Fast or irregular heartbeats
- Confusion
- Changes in mood or behavior
This is not a complete list and other side effects may occur. Talk with your doctor if serious side effects occur or if you have any concerns about new or worsening side effects.
Drug Interactions — Atypical Antidepressants
Again, because medications don’t fit into a single category, drug interactions might vary significantly. The list below is not meant to be complete:
- MAOIs: Risk of serotonin syndrome.
- Warfarin: Can increase the risk of bleeding.
- Antipsychotics: May increase side effects like tardive dyskinesia.
- Lithium: May require dosage adjustments due to interactions.
- Stimulants (such as amphetamine): Combining these medications may increase the risk of a seizure.
- Apalutamide (an androgen receptor inhibitor): This drug might also increase the risk of a seizure.
- Opioids (such as butorphanol): Individuals may be at a higher risk of a seizure when combining bupropion with opioids.
- Certain antibiotics (such as cycloserine): The risk of a seizure may increase.
- Certain cannabinoids (such as dronabinol): Combining bupropion with other drugs that may also cause seizures, such as dronabinol, may increase your risk of a seizure.
For a complete list of known interactions for a specific medication, refer to the Drugs.com Drug Interaction Checker.
Treating Depression with the Right Antidepressant

For millions of individuals, antidepressants put a higher quality of life within reach. These medications can be effective in increasing mood-regulating neurotransmitters in the brain, allowing you to feel happier and live your best life.
However, antidepressants are not without side effects, including the potential to increase thoughts of suicide. It’s important to share your side effects and any other concerns with your healthcare provider. Finding the right antidepressant can be a trial-and-error process, and working alongside your doctor can help you find the best fit for your condition.
Get the Lowest Price for Your Antidepressants
Save time and money on your depression medications (and all your other medications) with BidRX. Simply list your prescription and let pharmacies compete for your business. You can choose the bid that works for your budget and make medications more affordable than ever.
Create a free account, find your medication, and place your bid today!
This information is intended for general informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or medication.
